Throughout 2022, the Alberta Medical Association worked to draw attention to the care deficit that continues to delay and reduce access to essential care across the entire health care system. We’ve written several issue papers, including one on the mounting pressures in Alberta emergency departments and their impact on patients, and others on issues such as pediatric mental health and the drug poisoning crisis. Our most recent albertapatients survey, conducted in November 2022, showed that while some care deficit pressures are beginning to decline, many elements of the care deficit continue and have actually worsened since the survey was conducted in the spring of 2022.
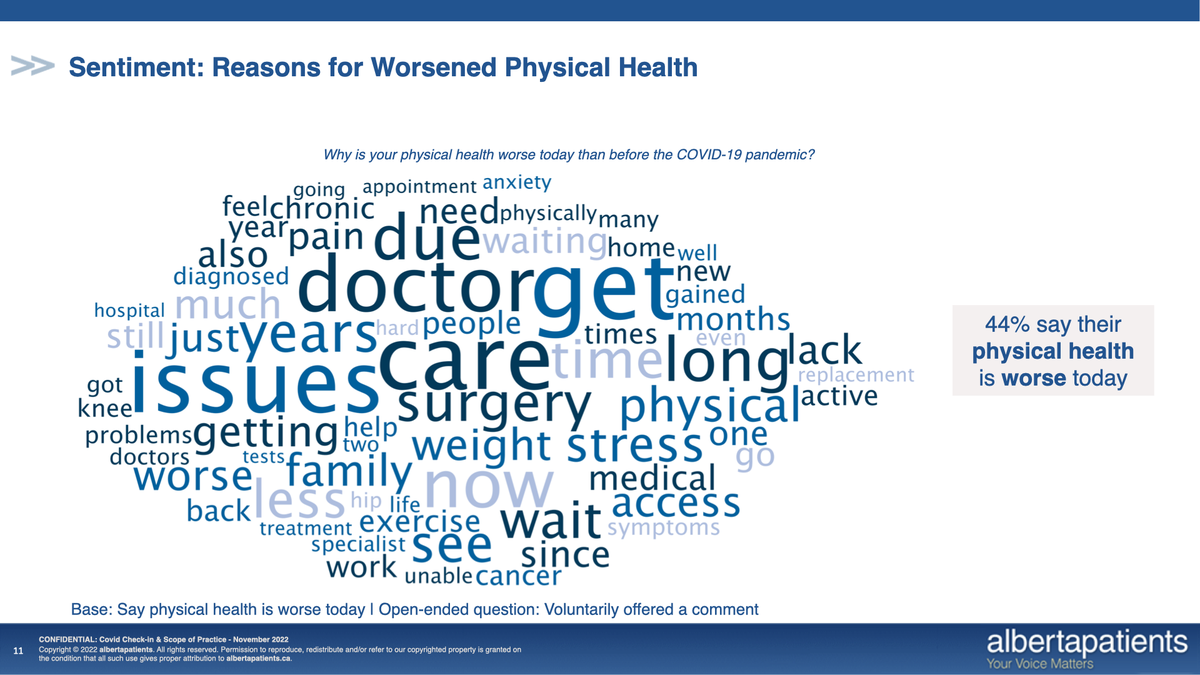
The November 2022 survey found that 44% patients say their physical health is worse today than before the COVID pandemic began, which represents a modest improvement since spring, when 48% reported a physical decline during COVID. In addition, mental health impacts have notably improved since the spring with 48% indicating they feel their mental health today is worse than it was prior to the start of the pandemic, representing a significant improvement since the spring survey when 65% reported negative mental health impacts. It’s a welcome step in the right direction.
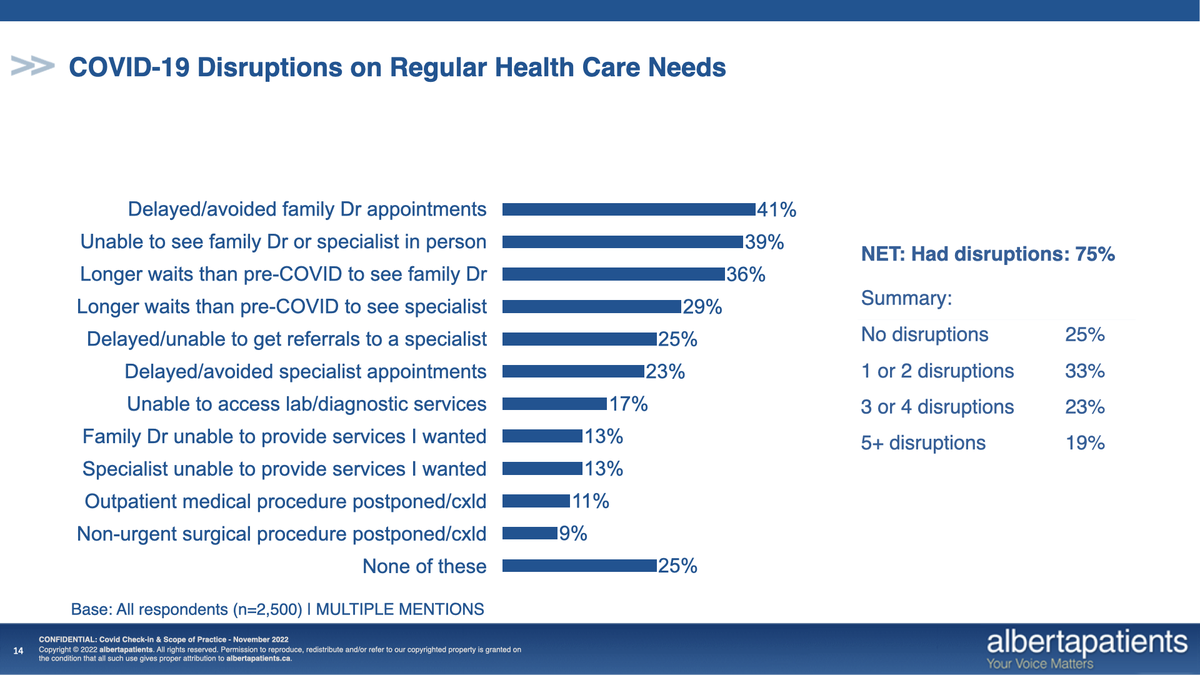
Unfortunately, despite these positive changes, there are still indications of notable care-deficit-related strains on our health care system. Access continues to be a growing concern for Albertans, with 41% reporting they have had delayed or missed appointments with their family physicians, while 23% report the same for specialist appointments. At the same time, 39% say they have been unable to see their physician in person and are experiencing significant wait times to see family doctors (36%) and specialists (29%). Front-line physicians advise that often the wait lists have become so long that in some instances new names are not being added.
So, what does this mean for Albertans? It means they are still facing delays in screening, tests and diagnoses. It means they are still waiting longer for care, treatments and surgical procedures. It means patients are still unable to see their family doctor for prescription refills or to follow up on test results and often they feel they have no other option than to head to Alberta’s increasingly overwhelmed emergency departments.
This continued reliance on emergency departments is especially worrisome as our province is dealing with an influenza season that hit early and hard, especially for children. Alberta’s pediatric emergency departments have been overwhelmed with young patients who have borne the worst of a combination of COVID-19, influenza and RSV.
In early December 2022, the AMA’s Section of Pediatrics issued a press release calling for stronger protective health measures to mitigate viral transmission. The Section of Emergency Medicine stated support for the pediatrics messages. These measures included recommending increased public messaging around the safety and efficacy of influenza and COVID-19 vaccines in children; increased accessibility to vaccines, especially amongst marginalized populations, by offering school vaccine clinics or mobile vaccine services; and a temporary mask requirement in schools for children and educators, along with the provision of high-quality medical-grade masks.
They also recommended the use of HEPA purifiers in classrooms, more emphasis on the importance of ventilation and filtration, encouraging frequent hand washing, and access to sanitizer and sanitization of high-touch surfaces in schools and essential indoor public spaces. In addition, Albertans were encouraged to stay home from work and school when sick.
We know our hospitals will continue to feel the strain of this influenza season for many weeks to come. Emergency rooms are pushed beyond capacity and waiting rooms are overflowing. Children up to the age of 19 account for nearly one-third of flu-related ICU admissions, according to provincial data.
This challenge is not unique to Alberta. In mid-December, B.C. Children’s Hospital approved double-bunking patients in single-occupancy rooms and the Ottawa Children’s Hospital called in the Canadian Red Cross. Here in Alberta, our situation is worsened by our low pediatric vaccine uptake. Alberta has one of the lowest pediatric influenza vaccine rates in the country, with only 15.5% of children between the ages of 0 to 11 years having received their flu shots. Flu is the second leading vaccine-preventable cause of death in Canada, which means vaccines can have a measurable impact. That’s why health experts across the country have been imploring parents to get themselves and their children vaccinated.
The impact of the viral season has already dramatically exacerbated Alberta’s care deficit. In early December 2022, the Rotary Flames House, a pediatric hospice in Calgary, paused its services and discharged respite patients in order to redeploy staff to Alberta Children's Hospital. Staff were also pulled from five of the facility's 82 outpatient clinics, meaning that the gastrointestinal, surgery, nephrology, orthopedic and pulmonary function clinics could see as much as a 50% reduction in services. Infectious disease experts warn that adult cases usually follow on the heels of the peak of the pediatric wave and that adult cases are expected to be more severe as well. This will, undoubtedly, further escalate the existing care deficit well into 2023.
The AMA will continue to survey Albertans to gather their experience and to advocate for ways to ease pressures so that people can get the care they need when they need it. It will take all of us, working together, to get through this care deficit crisis.
Banner image credit: Pixabay.com

