The Alberta Medical Association (AMA) should support members more in taking on the complex issues faced by physician leaders in developing higher quality of life for physicians who can then perform at their best. That is the basic opinion emerging from AMA’s Member Insight Survey earlier this year.
That survey outcome tracks with the AMA’s mission statement: “The AMA advances patient-centered, quality care by advocating for and supporting physician leadership and wellness.” The member feedback also highlighted the many challenges to be overcome in achieving this mission.
The AMA distributed the survey to approximately 14,000 members. The email invitation provided a link to TWI Surveys’ private and secure questionnaire located on the TWI server. As the third-party survey provider, TWI holds the data to ensure confidentiality and the anonymity of survey respondents.
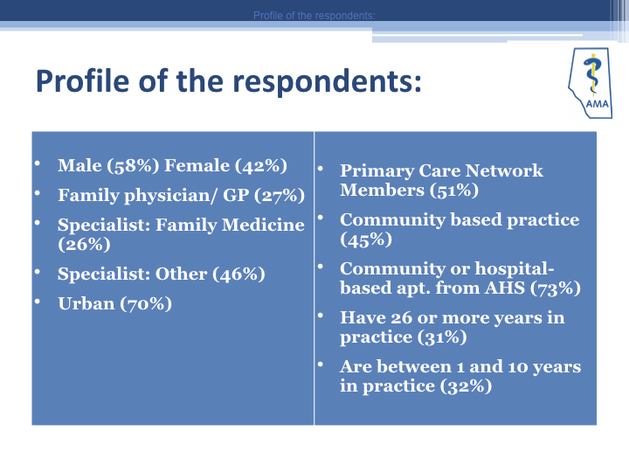
The survey was distributed on February 26 and closed on March 5. Responses were received from 1,339 members for a response rate of 10%. This is a typical response rate for this kind of survey and provides valid and reliable opinions of members. The data is valid 19 times out of 20 within a margin of error of +/- 2.55%.
The questions were selected to better understand individual member’s perspectives around issues facing the profession relating to access and quality for patients and to pressures in their practices. There were also open comment questions to hear members’ exact words and opinions.
Conclusions from Member Insight Survey
There is evidence that things are changing in the Alberta health care system. Parts of that system have been improved. For example, more collaborative care models have emerged and new ways of using technology have improved access to care.
As a professional body, physicians report holding unifying beliefs and values. With a clear vision for the future, the evidence of progress and physicians’ shared values can provide optimism for those who seek to lead the effort for further advancements.
Those leaders will be confronted with a difficult set of variables to manage and overcome. Physicians are burned out from change fatigue, increased patient volume, more complex demands, increased regulation and financial pressures. Most physicians lack the capacity to take on significant system changes.
Physicians vary in what they believe are effective strategies to accomplish quality and sustainable care. Is it a payment model, a care model or a management model – or all three? With each announced change, the physician role and the process for assessing and caring for patients is impacted.
Trust is critical to leadership, but not all of the essential partners in the system are trusted by some members. The AMA has earned the trust of most but not all members. Alberta Health Services is not trusted by many members: a member may say, “They don’t understand us, they are not competent to manage clinical care, and they aren’t believable.”
It is difficult work to align and transform a complex system like health care in Alberta. According to members, transformation needs to be done. The current state of the system is not providing the best care and is not sustainable for practitioners. Collaboration and innovation will be required. Scarcity of resources, the need for efficiency, and old patterns of behavior will need to be addressed.
What members said
Members shared their opinions that the Alberta health system has the following:
- More complex patients (aging, options for care, opioids)
- A staid financial model that is still primarily fee-for-service
- More and more specialized care
- Fragmented communication opportunities
- Many burned out physicians
Results show these beliefs are common among most members:
- Patient outcomes matter.
- Quality of care is important.
- They would like to feel valued by patients, colleagues and other health care stakeholders.
How the health system and change affect members
Our values shape how we experience the world. Physicians are no different, and with the current work environment, some critical values for physicians will continue to be challenged. Three significant challenges to achieving positive change exist.
Autonomy – who manages clinical decisions and who can make those decisions- Pharmacies, PCNs, other clinic options, and roles of nurse practitioners are challenging historical roles and protocols.
- These examples bring varied member responses from positive progress to outright resistance.
- Fair compensation
- Acknowledgement of increased costs
- Responsibility held by a physician
- How others are paid in the health system
One physician may declare we need a fee-for-service or productivity will drop and put patients at risk. Another physician will highlight the need for more nursing support. Another physician notes that to be sustainable a fee-for-service model requires that simple care act as a financial offset to treatment of more complex patient care. Autonomy, recognition and achieving outcomes are values that enable or frustrate the strategies that improve care and the work environment of physicians.
As in any profession, individuals come with ideological beliefs: some look to the market for solutions, while others would look to the bureaucracy to hold the responsibility for the work environment. Physicians would agree that they want to provide the best care for their patients.
In 1997, the AMA was jubilant when it negotiated a Master Agreement with the provincial government. After that milestone achievement, TWI was asked to review, summarize and gather feedback from members about the Master Agreement. After ratification, it became abundantly clear that members did not feel the same way. The Representative Forum not only reviewed and adopted recommendations, it applied significant resources and reflection to ensure this gap in expectation would not happen again.
The Master Agreement review led to 20 years of surveys, focus groups and member outreach, which all reflect the opinion that the health care system can be slow in changing. In the last couple of years, however, members shared their opinion that some things have changed:
- Physicians are dealing with oversupply in some regions of the province, while undersupply is a reality for other regions.
- Continuity of care is difficult to achieve.
- EMRs are adopted, while other technologies have emerged.
- More physicians would consider being an employee with salary and benefits.
- Physician burnout seems to be more pervasive.
Progress, new challenges and systemic issues are the reality. The purpose for members is clear. The AMA should support members in taking on the complex issues as physician leaders to produce a higher quality of life that supports physicians to perform at their best. Members should know they have similar values and desire the same end state. Dialogue, curiosity and experience will be required to advance toward those goals. To be successful, members will benefit from affirming their leadership, recognizing contributions of their leadership and tracking demonstrable results.
For a more information, download the complete results here.
