As the first wave of the COVID-19 pandemic crests, without a vaccine, it is an opportune time to briefly revisit and learn from the 1918-19 Spanish Flu.
My earliest recollection came in the 1970s, when infectious disease experts were prophesizing that a pandemic was already overdue. Since then, researchers have sequenced the 1918 virus (2011), and Newfoundland’s Mark Humphries has postulated (2014) that the pandemic originated in northern China in November 1917 and not in the army camps in Kansas, USA, or in France.
In early 1918, 25,000 Chinese laborers crossed Canada in sealed trains heading to the European front. About 3,000 became ill and were quarantined in Canada. More died in Britain and in France before they reached the front. In April 1918, the first wave began with one-in-five soldiers in allied and axis armies developing the flu. The German Field Marshal, Eric Ludendorff, blamed it for blunting his spring offensive. The second wave came in September and was much worse.
The 1918-19 Spanish Flu in Alberta
The government was 13 years old and only partially ready. It had maintained the Northwest Territories public health structure, initiated after the 1870 smallpox epidemic. A board of public health and a medical officer of health were appointed in 1906. The MOH was Dr. William C. Laidlaw (1912-26) but he was overseas in the Canadian Army Medical Corps. His duties were assigned to the 1907 appointed Edmonton MOH, Dr. Thomas H. Whitelaw. The only other full-time MOH, was Calgary’s Dr. Cecil S. Mahood. Part-time MOHs were appointed in some smaller towns.
By the time the infection was over, Alberta would officially record 38,308 cases with 4,380 deaths (cf. 40,000 to 60,000 deaths in Canada) in a population of 500,000. Many felt this under-reported the cases.
In Calgary
The first wave arrived in Calgary on October 2, 1918. It lasted 51 days and was followed by a second wave starting December 11 that lasted 47 days. The third wave lasted a month and ended April 25, 1919. Each wave had fewer cases, but higher death rates. Clinically, the flu cases presented with a temperature of 101-103 degrees F, fatigue, coughing and signs of an upper respiratory infection. Sometimes it came on so rapidly the patient collapsed while out walking. The fatigue lasted up to 14 days. Recovery (or death from pneumonia) usually came in seven days. Most of those affected were 20 to 40 years of age. Houses were quarantined with a placard placed in the window, although not everyone chose to flag their homes.
The first cases likely arrived on a 3 a.m. troop train. Forewarned by a telegram from Regina, Dr. Mahood transferred 15 infected soldiers to Camp Sarcee. Within five days, two registered nurses and a soldier were infected. Ten days later the flu had spread so rapidly, Dr. Mahood banned gatherings at churches, schools, theaters and in public places. The Public Health Act was amended on October 16 to cover the epidemic. Courts were closed on October 18. Masks were required on trains and streetcars before becoming mandatory when outside on October 25. Some were labelled “buy a bond” to support war bond purchases. Medical students rode the rails to ensure compliance and many people were fined for non-compliance.
Then on October 30, all non-essential stores were closed, although some offered telephone-ordered goods for front door pick up. The community response was not unanimous. Some churches circulated pamphlets condemning their closure.
Spirited volunteers organized themselves to check on neighbors, and bring them food and water. Free food kitchens sprang up. Children who had lost their parents and didn’t have relatives were admitted to a shelter, pending an adoption. Hospital emergency departments triaged patients to three schools, the old Calgary General Hospital and a church. Hotels donated beds and sheets; the Red Cross – masks.
On November 4, Dr. Mahood felt obligated to release a “cheer up” message. The same day the business-orientated city council voided Dr. Mahood’s orders, but the board of health intervened and backed Dr. Mahood. Then on November 11, the Armistice ended WWI. A celebratory “solemn thanksgiving” was planned for November 17, but was cancelled by Lieutenant Governor Dr. Robert G. Brett. Many were still held, followed by another round of infections. The first wave ended as abruptly as it began, on November 23, with no new cases being recorded. Stores immediately reopened.
Elsewhere in the province
The infection spread to Edmonton by October 16. The high wartime enlistment rate had already denuded the province of one-third of its 400 doctors, along with many nurses. Caregivers in the north were particularly short staffed, with only three doctors in the northeast part of the province. The government responded by appointing the Minister of Municipal Affairs, Alexander G. MacKay, as responsible for the new (second in Canada) public health department in early 1919. He sent 200 health care staff to help in the north. Unfortunately, his work was cut short when he died in 1920 from cardiac complications secondary to the flu.
Physicians were affected, too. At least one died and Dr. George D. Stanley almost did. Dr. Malcolm R. Bow in Regina noted that their 30 doctors were reduced to 10 who could still work. The list of prescriptions was limited. The commonest were for opiates and aspirin. Stores advertised up to 25 patent medications including camphor gum, Epsom salts and castor oil. Physicians who prescribed pharmacy-filled liquor orders found their patient volumes increased. Gouging included raising the price of a coffin by $12. Registered nurses were criticized for double-billing when they charged for their overtime work.
While the 1918-19 flu epidemic recorded over 38,000 cases (cf. over 6,000 positives so far with COVID-19) the major burden fell on cities, towns, families and individuals – without assistance from the federal or provincial governments. Treatment was limited to isolation attempts, masks and tolerance, as it ran rampant. Testing, contact tracing and medicare did not exist.
The postwar impact on health care
Anticipating the postwar need for more laboratory testing, Drs. H. Marshall Tory and Allan C. Rankin recruited Dr. James J. Ower (the future University of Alberta Dean of Medicine), a serologist and pathologist, to come to Alberta and support the creation of the first VD clinic in Canada in 1919. Foreseeing an increase in university enrolment after the war, U of A president Dr. Tory initiated a pharmacy school (1915) and a dental school (1918).
His most important decision stemmed from the wartime shortage of doctors to care for flu patients and the conclusion that only half the doctors who finished their last two years at eastern medical schools returned to Alberta. Despite being overseas managing the Khaki University, Dr. Tory proposed increasing the three year MD program to five years. Approved, his proposal was cemented when he secured a Rockefeller Foundation conditional grant of $500,000 in early 1920, subject to completing the government approved new medical school building and graduating MDs. He immediately appointed Dr. Rankin as the dean. The faculty graduated the first MDs in 1925 and dentists in 1927.
To prepare for the expected flood of wounded veterans, the province approved taxing properties to pay for the new municipal hospitals starting in 1917-18. The first hospital originated in the border town of Lloydminster. Soon, multiple municipal hospitals extended across rural Alberta and Saskatchewan.
To fill the continuing care void in northern Alberta, MacKay began the District Nurse program in 1919, sending the first nurses to Peace River that year. It was the second such program in Canada.
The belief that a public health system was essential – and prevention, especially through vaccination was a requirement – led to the creation of a ministry of health (1923). Alberta would be the first to build a polio hospital in Canada (1928), provide free polio rehabilitation, and introduce the second free TB act in Canada.
Postwar politics changed too
Agrarian unrest on the prairies had increased during the war. Wartime inflation increased the cost of living by 50%. So in 1919, the frustrated agriculture movement formed its own political party, the United Farmers of Alberta. They won the 1921 election, holding power for the next 14 years.
One major focus was on health care. UFA president Irene Parlby declared health care to be a right in 1919. That year, she admonished the profession for not providing returning physicians with refresher courses. Appointed the UFA Minister without Portfolio in 1921, she became the strongest supporter of Health and Agriculture Minister, George Hoadley (1923-35). They would lead the movement for government involvement in improving access to care through a health insurance program. It culminated in the passing of the first medically acceptable, government subsidized health insurance act in Canada in 1934.

And now
Despite more than 100 years of anticipation, the world has been caught short by COVID-19. More disturbingly, there is neither a safe and effective vaccine, nor is one anticipated for at least a year. That leaves only one approach: focusing on containment and management through isolation, social distancing and testing to determine positive cases or immunity before a staged return to normality.
We live in a world with increasing globalization, travel, interdependence, international supply lines, and rapid movement of people (and the virus). As such, a coordinated, research-validated, rapid response has become an imperative. Surprisingly, epidemics during the past 100 years – including SARS (2003), H1N1/swine (2009), MERS (2012) and Ebola (2014), Zika (2015) – have not been a sufficient stimulus to create an effective early warning and containment system. Nor are there vaccine platforms on the shelf to reduce the year or more timeframe to confirm they are safe and effective.
While a spectrum of antivirals have evolved following the HIV infection in the 1980s, and artificial intelligence has created a shortlist of other compounds worthy of study, the damage has already been done. The worldwide financial cost (more than $8 trillion) and human cost (now more than 200,000 deaths) have become enormous and are still rising, all before factoring in the likelihood of more waves and more virulent infections.
The world has been thrust into a recession and possible depression rivalling the 1930s. Some will say it was avoidable, or at least could have been attenuated. Canada can provide leadership in the development of an international approach to shorten the current epidemic and reduce the likelihood of a future COVID sequel.
Will we?
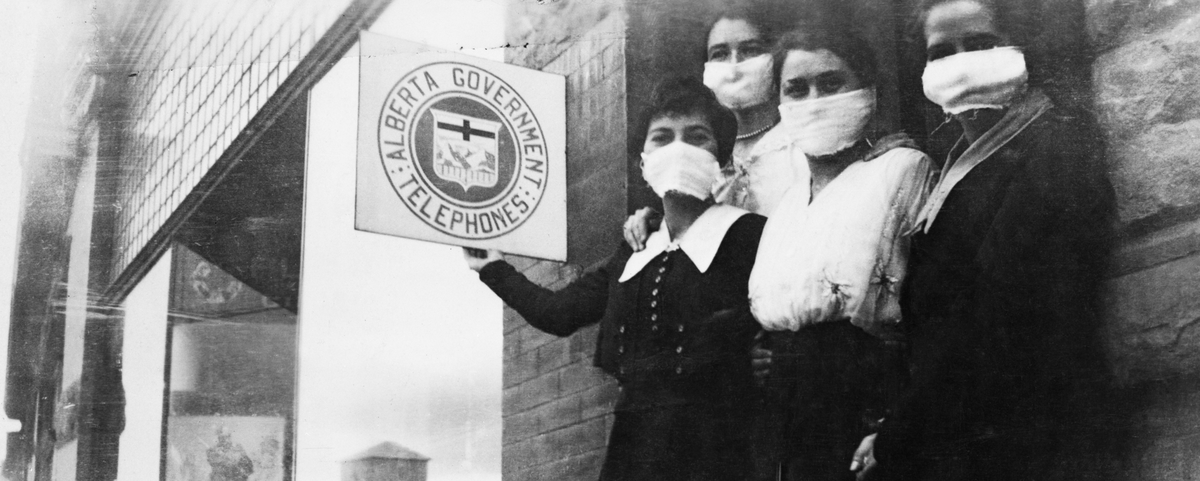
Banner photo: Canadian Bank of Commerce staff, during Spanish flu epidemic, Calgary, AB. (Photo credit: Glenbow Archives, Archives and Special Collections, University of Calgary)
