As an assessment physician with AMA’s Physician and Family Support Program (PFSP) Assistance Line, “stressed … burnt out … overwhelmed … depressed” are words I hear multiple times a day during the weeks I’m on call. In 2020, calls to access support for mental health concerns overtook the most common reason for calling in past years (support for family and relationship issues), and mental health concerns represented 46% of all calls to the line.
Pre-pandemic data on the well-being of Canadian physicians similarly indicated that despite the vast majority of us scoring high on measures of resilience, 30% of us are burnt out, slightly more than that are depressed, and 8% of us considered suicide in the 12 months preceding the survey. Resilience only takes us so far.
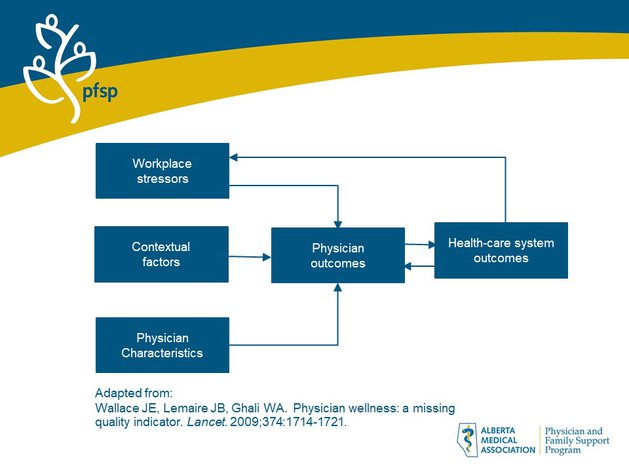
The diagram, a schematic based on an important paper on the significance of physician wellness published in The Lancet, illustrates the empirically validated relationships between contributors (on the left) to negative physician outcomes (near the center) as well as the effects of them on our health care system (on the right). Our wellness matters, not only to ourselves and our families. We know from experience as well as research that 80% of physician burnout (“I’m tired, I feel ineffective, and I don’t care anymore”) can be attributed to system factors, some of which we can’t directly change. Peer support, however, can buffer us from burnout and promote a more just and supportive culture within which we can more easily flourish.
To flourish requires experiencing not only positive feelings of satisfaction in providing good care, of reward from interactions with patients and of contributions to positive patient health outcomes; we must also acknowledge and work through the distress or even secondary trauma we experience when patients have adverse events, when we make errors resulting in patient harm, or when our patients don’t get better, or they die.
How often do we reflect on how we are impacted by these events or by the cumulative effects of difficult situations in our daily work caring for patients with treatment-resistant or chronic illness or by having to make choices in the face of legitimate competing priorities or values? The fact that these experiences come with the job can lead us to dismiss their psychological impact, perhaps until anxiety, burnout or depression demand our attention. It is the emotional demands of our work that have the strongest negative relationship with physicians’ well-being, not the number of hours spent working, or the conflict between work and family life, or even work overload (though the latter was also found to negatively influence well-being). Yet we are ill-prepared by our training and the culture we practice in to deal with the emotional impact.
While PFSP is the most utilized physician health program in the country, only 15% of Canadian physicians reported accessing a physician health program in the five years preceding the Canadian Medical Association’s National Physician Health Survey published in 2018. Physicians perceive barriers to seeking support such as believing that the situation isn’t serious enough, shame/fear of being stigmatized, lack of time, concern about confidentiality, and uncertainty about how to access support.
Acknowledging these barriers, one of the most important findings from research is that physicians prefer to seek support for stressful situations from physician colleagues. Guided by these findings, the first formal one-on-one physician peer support program was launched in 2006 at Brigham and Women’s Hospital (BWH) in Boston under the leadership of Dr. Jo Shapiro.
Peer support in medicine is both formal and informal, and both are alive and active right here in Alberta. AMA’s PFSP Assistance Line has been providing confidential physician-to-physician peer support for over 20 years. Medical leaders approached Well Doc Alberta (WDA) for guidance on how to best help physicians in need of support. Thanks to the leadership of WDA, peer support team training based on the BWH gold standard model has been available in Alberta since 2018. Intact physician groups interested in implementing a one-on-one peer support program in their practice can contact WDA for training.
Trained peer supporters listen and help reflect, honor, validate, and sometimes reframe and make sense of the experiences of their colleagues. Peer supporters ascertain how the physicians are coping and facilitate access to the next level of support when desired, via PFSP. The physician needing support can call the 24/7 PFSP Assistance Line to talk further about resources available, including professional therapists. Peer supporters are “the help to get the help” for colleagues. Assessment physicians at the PFSP line are also available to peer supporters to discuss confidentially concerns or questions that arise from their unique role. For docs supporting docs, we’ve got your back too.
Beyond formal programs – and of equal importance – in the hallways of our medical homes, each of us can be of support, providing “emotional first aid” to a colleague in the midst or aftermath of an adverse event, or just checking in with someone having a tough day. Better yet, proactively saying to a trusted colleague: “Will you let me know if you see something about me that makes you concerned that I’m not well? And I’ll do the same for you?” This is how medical culture changes from the inside. From one of shame and blame and suffering in silence to one that accepts our vulnerability and supports us in taking care of ourselves so that we can get back to doing what we do best.
The growth of peer support in all of these forms makes support accessible, part of a caring medical culture that, rather than denying and stigmatizing physicians’ need for support, takes seriously the emotional impact of our work, sometimes at the time and place we experience it. Peer support removes barriers to accessing what we need to stay well or get well and does so in the way we want to be supported. Support for us, by us, buffers us from burnout, increases our resilience and leaves us less distressed. Just what the doctor ordered.
Recommended reading
Helping each other through the pandemic: providing informal physician-to-physician peer support
5 Things to Know About Peer Support
The CMA Wellness Hub, Peer Support section
Guide to help people recognize signs of distress in physicians
The Well-Being of Medical Relationships
Banner image: Sasin Tipchai, Pixabay.com

